Document with Confidence and Protect Your Nursing Practice
Accurate, clear records safeguard you and your patients.
This is for you if you write patient or client notes. And that’s everyone.
How will your nursing notes defend you if a patient, relative, coroner/ME (Medical Examiner) or anyone else made a complaint against you or your team?
Think about it. Rock-solid documentation could literally save your career.
It’s about a 10-minute read, so…buckle up and be prepared to critique your patient note making.
During the pandemic I was working on a busy ward. One of my patients was a lady in a side room, and I looked after her for three or four shifts. Each day I was working with her, I offered her a shower, promised it would be clean, and that I could wheel her through to the bathroom so she wouldn’t be tired. I offered to wash her hair, and she’d feel better.
Each day, she declined.
About two weeks after she went home, the ward manager asked us if they remembered the lady. She’d had a complaint from the husband saying, in the time his wife had been on the ward, she hadn’t had a bath or a shower.
I explained my shower offers when I’d looked after her, but guess what? I hadn’t documented them. If I had, my manager could have answered the complaint more quickly.
The details of care matter.
You’ve spent how many years studying to be a nurse? It’s your income, which means it pays your bills, rent, mortgage, and for many of us, nursing is our identity.
Imagine having that taken away in a heartbeat because you couldn’t prove you did the right thing, or if you did the wrong thing, you did it for the right reasons.
It happens. Careers and reputations are destroyed because someone had an axe to grind and proved their point better than the nurse could defend hers.
Remember, if someone makes a complaint, they are criticising the care you’ve given. Your note-taking/documentation will help to defend you if this happens.
In this newsletter, we’ll look at:
What is documentation (seems obvious, but let’s get it defined)?
What is defensible documentation?
Why does it need to be defensible?
How to write objectively and professionally.
In all that, we need to think about:
1. Who might read our notes.
2. Why they might read our notes.
3. So, what do we need to write for them, and for ourselves?
Off we go.
If someone makes a complaint, it may be justified – things should have been different and whatever happened fell short of their expectations. Perhaps they should have been different because there should have been more staff on the shift, or because the equipment should have been working properly.
Even if there are circumstances beyond your control (staffing levels/equipment maintenance/other patients), these need to be documented objectively. This means anyone reading your notes has a full picture of what else was happening when something went wrong for their loved one.
What is documentation?
Our nursing and medical documentation includes anything that contains patient details. This is anything digital or on paper.
Think of care plans, X-rays, scans, ECGs, other device print-outs (eg from intensive care machines, telemetry etc), medicine charts (MARs), paper letters to and from any member of the healthcare team, social workers, community teams, pharmacists, specialists in other districts. But also emails, text messages and other correspondence.
If you’re in doubt about whether it’s a “medical/nursing document”, ask yourself if it has (or should have) patient identifiable information on it. If it has, it relates to that person and needs to be treated as confidential. It’s patient documentation.
We’re going to focus on anything you write about a patient. It’s up to you whether you want to help others improve their documentation skills, but when all team members document well, everyone wins.
Your documentation isn’t just there to protect you; its other primary role is to communicate to the wider team. That means if someone else is going to read it and make use of what you’ve written, it needs to be laid out well.
What is defensible documentation?
Defensible documentation is just good quality documentation. It’s thorough, detailed and reflects good quality care. But more than that.
When I write these letters to you, I try and arrange the text so it’s easy to read on a screen. If you type onto a computer for others to read on a screen, then leave plenty of white space, because a dense block of text is off-putting to read.
If you write by hand on paper, don’t write one long paragraph – use the lines. Just score through any extra space or lines. For example, if I’m writing by hand and have finished my point in the middle of a line, I’d draw a line: -----------------------------------to the page margin.
This is so extra text can’t be added after the fact.
On paper and digital, you can use bullet points, headings, etc. Good quality documentation makes the text clear, accessible and useful to the next reader.
When we think about who the reader is, it’s probably more people than you’d imagine. Immediate colleagues are the obvious first thought. But, depending on where you work and your healthcare system, auditors, commissioners of services, researchers, healthcare professionals from other units, specialities and departments will want to read them too.
We’re writing for someone who’s not there with us.
Of course, we also need to think of patients themselves, family members and their legal representatives who may want, or have reason to read them.
So, when we write, we write for all of these groups, but that’s not as difficult as it sounds.
Nurses regularly communicate with senior colleagues, other HCP disciplines, patients and families about the complexities of patient care. This means if we can say it so they understand it, we can write it so they understand it.
Write in simple language that both the patient and the senior specialist colleague will understand. Long words, technical and jargon-filled language just makes us look like we’re showing off. And if it sounds clever but we can’t explain it in simple terms, we don’t understand it well enough.
Why does it need to be defensible?
I said at the top of the page that for many, nursing is more than a job, it’s an identity, a way of life. Many have gone from school to nursing school and into the nursing profession. As an income provider, nursing/care might be all we’ve ever done.
Others come to care and nursing after careers in other areas.
Imagine then, having that career taken from you because you lost your nurse registration. Good documentation defends us when someone makes a complaint about the care we’ve given. If that complaint is serious, it could mean our licence to practice could be taken away.
When our documentation is detailed and answers questions someone might have about what happened, a complainant will move on to someone whose notes are weak and have gaps.
Defensible documentation not only communicates to our colleagues, it defends us individually and as healthcare teams. If everyone’s notes are strong, there’s less opportunity for a complaint to be upheld.
How to write objectively and professionally.
This could be a long section, so let’s think about this as three (more) questions you can think of as you write your documentation.
1. Am I being objective? Being objective is about keeping emotion and emotive words out of our records, sticking to the facts, and not giving an opinion unless we’re qualified to give it.
For example, if you’re recording what Donny ate for lunch, you could say “Patient ate some of his lunch, I don’t think he was hungry.”
But this doesn’t tell us much. It would be better to say something like:
“Donny was given steak, chips and peas for lunch. He ate a few of the chips and half the peas but none of the steak. I asked why he didn’t want more, he said he’s a vegetarian and his dentures are at home, but also that he isn’t hungry today.”
It’s longer, but tells us what we need to know about what Donny needs – his dentures and a vegetarian meal.
The first note also talks about what you think (that he wasn’t hungry) – how do you know if you didn’t ask? The second note has the facts of what he was given, what he ate and why.
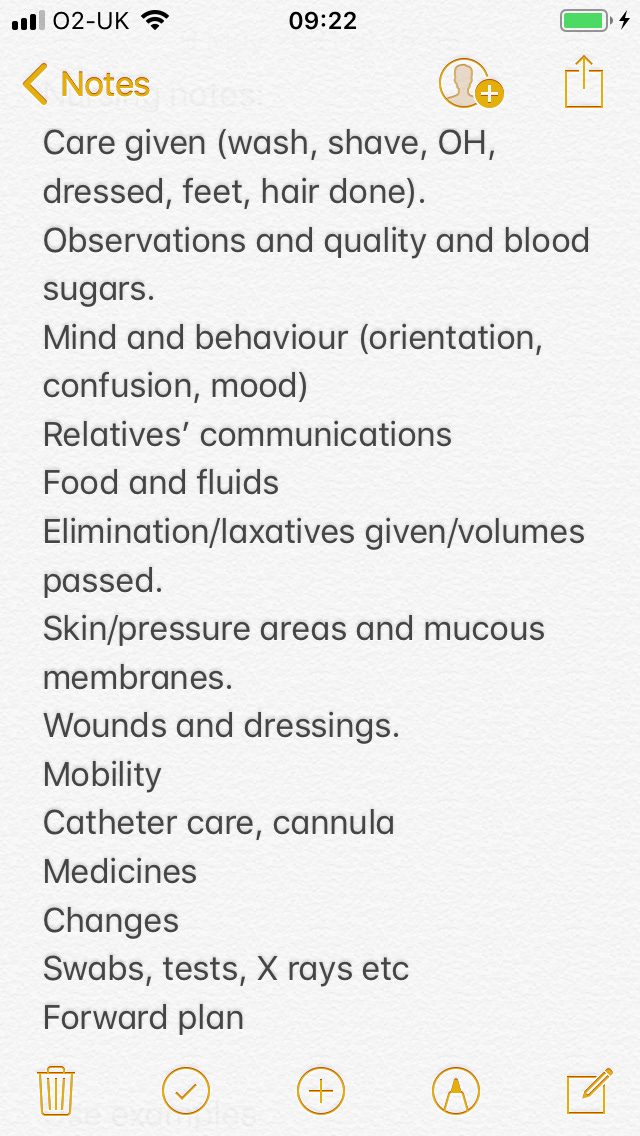
2. Do my notes include everything that needs to be included? I don’t know about you, but I can’t remember everything I’ve done. So after the incident described above, I made a note on my phone about the patient’s activities of daily living (ADLs) and used this as a reminder to write about each.
(OH = oral hygiene)
3. When might something that happened today become important? It’s easy to get lost in the weeds with this one, but think about it from three positions:
a. What if the patient read my notes, would they agree with what I’ve written?
b. What if a colleague – a physical/physiotherapist, a doctor, a nurse/specialist from another discipline – would they get all the info they need?
c. What if a lawyer read my notes? Would they get the answers they need and what criticisms would they have about my care?
Last thoughts.
This is a big topic, but remember that when you create your notes and documentation, you’re communicating to your colleagues but also to your future self.
Tomorrow, you won’t remember what happened on your shift today, so write it before you forget it, write it fully, and make it clear so it’s easily read.
Happy documenting, and until next week,
All the best,
Elspeth.