This is for you if you look after people with back pain or have had back pain. There are a few red flags that we need to look out for.
It’s about an 8-minute read with links throughout, as usual.
Your patient, let’s call her Sarah, complains of pain in one side of her butt. It’s not just in her butt, it’s going down her leg and it’s really, really painful. She’s struggling to walk, sit, or do much of anything.
She says it’s happened before and she knows what it is. It burns, and tingles like pins and needles, and at some point, her leg is going to feel so weak that she might fall.
Nerves. They tell us everything about what’s going on outside and inside us. Where would we be without them?
And boy, do they let us know when something’s wrong.
Sarah’s experience tells her this is sciatica. Its presentation as pain in one buttock and one leg is characteristic. Because she’s in pain and knows potentially what’s coming, she needs reassurance and care.
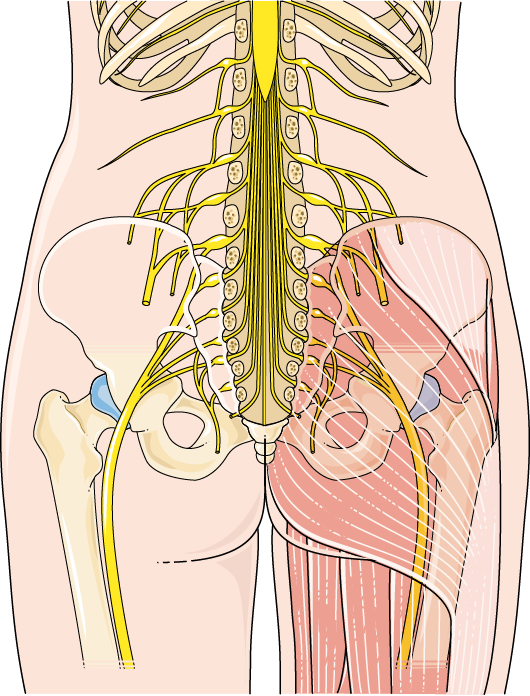
With one on each side (obviously), the sciatic nerve is a long, thick nerve, running from the pelvis to the knee. Past the knees, they split into nerves that serve the lower legs, ankles and feet.
If the nerve gets pinched, compressed, irritated or damaged, that’s where the trouble starts.
The pain is different from other types of back pain because it also affects the leg.
What causes sciatic damage/irritation/compression?
Look at the picture below, and you’re probably familiar with the discs between each of the bones of the spine. If one of the discs slips out of its position, it can rest on a nerve near it.
This is called ‘herniation’. A hernia is simply something (tissue or an organ) that protrudes through an opening.
So, disc herniation is one cause. This is also called a ‘slipped disc’.
Another cause is spinal stenosis, which is a narrowing in the channels the nerves pass through. Stenosis is from a Greek word meaning ‘to make narrow’. This means the channel can pinch the nerve, causing pain and disordered sensations.
Spondylolisthesis (say ‘spondil-oliss-theessiss’) means a spinal bone has slipped out of position, and this is touching or pressing the sciatic nerve.
Another back injury may cause it, including wear and tear to the bones and discs.
Who gets sciatica?
Sciatica is very common. It’s thought about 40% of people in the US will get it, and about the same number in the UK.
It affects people mostly between the ages of 30 and 50 years.
There are some risk factors, like: being overweight/obese, because the spine is carrying an extra load; being inactive; not having good core strength to support the spine; having a job with a lot of bending and lifting and not using good technique with lifting; and smoking.
Symptoms
Just as Sarah described above, the main symptoms are:
Pain in the buttock, extending down one leg
The pain is usually described as a burning sensation
Numbness
Tingling
Pins and needles
And just as Sarah described, it can come back if you’ve had it before.
Is sciatica serious?
For the person in pain, it is definitely serious. They need support and recognition of the difficulty they’re having and how everyday life is affected.
Pain breeds anxiety, and anxiety tightens the muscles, creating more pain. Sarah will be anxious about moving, about dealing with life, about sleep.
When you’re in pain, you don’t want to eat well and look after yourself, or drink plenty, because that means you’re going to have to get up and go to the toilet. This in turn can lead to urinary tract infections, dizziness, confusion and falls in the vulnerable.
It is a condition that’s manageable with the right approach, but there are some red flags that we need to be aware of: questions to be asked sooner rather than later.
These are:
Do you have sciatica on both sides?
Is the weakness or numbness in both legs severe or getting worse?
Is there numbness around or under your genitals, or around your bottom (anus)?
Do you find it hard to start peeing?
Are you unable to pee or can’t control when you pee? (If this is not normal for the patient. Remember, some people are incontinent to some degree.)
Are you able to poo normally? When you poo, are you able to control it as normal? (again, find out what’s normal for the patient.)
These could be symptoms of a serious back problem that needs to be quickly escalated to a specialist, as they could indicate damage to other nerves.
The nurse’s role in sciatica
We mentioned above that it’s important to support the patient. If she’s had sciatica before, ask what’s worked and what hasn’t – the patient is the expert.
Margo McCaffery, a highly recognised nurse and pioneer pain educator, defined pain as “… whatever the experiencing person says it is, existing whenever he/she says it does.”
Always remember this, even when others have judged the patient as ‘faking it’. People have many ways of managing their pain, including trying to sleep to escape it. Imagine not being believed when you’re in agony.
Be alert to the red flags mentioned above.
Pain that’s getting worse, or isn’t being lessened or resolved by the prescribed analgesia and other therapy, must be addressed and escalated.
If the patient hasn’t had it before, education is a way to reassure them. However, check they’re able to take in any information you give them, because someone in pain isn’t the best learner. And ask how they like their info – is a leaflet ok? Can you point them to a good video explaining the condition and its treatment? Is there a good website that’ll help?
Support and encouragement with doing the exercises prescribed for sciatica is important, both in shortening this ‘attack’ and in preventing it happening again. They will need to continue these at home.
In addition, taking regular pain meds will make the stretching exercises easier. A lot of analgesics make people constipated, so be proactive about asking about bowel habit.
Poop, as an aside
Never just ask, ‘Have you been for a poo today?’ This sort of question invites a ‘yes’ or ‘no’ answer.
A few days of passing only little pieces of stool (Type 1, on the Bristol Stool Chart), or having to strain to pass a stool, is a sign of constipation and can become serious.
Has the patient been prescribed and given laxatives as well as foods high in fibre, and are they drinking plenty of fluid?
Treatment for sciatica
As we’ve said, painkillers are the first-line treatment for sciatica. These may be analgesics, as well as a non-pharma approach, with things like heat packs and/or ice packs. Use these safely so as not to cause tissue damage.
The temptation is to rest in bed until the pain goes, but this can be counterproductive. So, unless a physical/physiotherapist has specifically prescribed rest, encourage the patient to be as active as they can, and to do the recommended stretching exercises.
Gentle stretches are demonstrated in the video here:
When the patient is out of pain and feeling more confident, it may be appropriate to discuss things like weight loss and lifestyle considerations – things like smoking, jobs and lifting etc.
Last thoughts.
Think about the last time you were in pain, even just a bad headache. Pain can really narrow your view of what you can do or even want to do, so empathy with the patient can be enormously therapeutic.
Because of the lifting and work nurses’ backs do, don’t forget we’re at risk of back injuries and sciatica. So:
Don’t let people rush you when you’re trying to manage a patient.
Use the right hoists and lifts.
Use the right technique.
Have good posture at the computer or when sitting.
Get people to help you with lifting and manual handling.
If your uniform stops you from doing your job comfortably, do something about it. Get a better size, complain to those who can change the shape or style: be a squeaky wheel. (When I was a baby nurse, we had to wear paper hats and the women couldn’t wear trousers – I still shake my head in disbelief).
Manage your own weight if you need to. Stay active and eat healthily.
Smoking? Need I say more?
You need your back long after your patients have finished with it. Take care of it.
Until next week,
All the best,
Elspeth.